Second in a series
The Philippines is one of the eight countries involved in the Asean Costs in Oncology (Action) study. Of the 9,513 total patients who participated in the Southeast Asian study, it represented 10 percent or 909 patients.
One of these patients was 61-year-old Marites (not her real name), single and living with her sister. She was 58 when she was diagnosed with Stage 3B ductal carcinoma, an inflammatory breast cancer.
This was the story Marites recounted:
“When I was told I had carcinoma, I did not understand that it refers to cancer and that I had a malignant tumor. I asked my family, relatives and friends. I even searched online about the diagnosis. I also sought medical advice from doctors who explained to me their treatment plan.”
Through mastectomy, Marites had her left breast removed. This was followed by chemotherapy and radiotherapy. Her tests showed she was ER/PR (estrogen receptor/progesterone receptor) positive and HER2 (human epidermal growth factor receptor 2) negative.
WebMD says that if your breast cancer has significant number of receptors for either estrogen or progesterone, it’s considered hormone receptor positive. Tumors that are ER/PR positive are most likely to respond to hormone therapy. HER2 is the one gene that can play a role in the development of cancer, according to breastcancer.org.
Marites paid for her surgery out of her savings and from the sale of the small property she inherited from her dead parents. Her uncles and aunts also helped her pay the treatment by remortgaging their homes.
Her cousin, a doctor, was the one who provided most of the medical supplies needed for her operation. She also received financial support from the Philippine Charity Sweepstakes Office through her daily radiotherapy sessions for one month.
Her cancer prevented Marites from continuing to work—selling insurance policies—and left her dependent on her brother and sister. After her treatment, she has been able to gradually practice ballroom dancing and nonrigid exercises. She, however, is unable to work again.
“My only wish is for the government to allocate budget for free cancer medical services because there are many poor and sick Filipinos who need assistance,” Marites stressed.
Subject profile
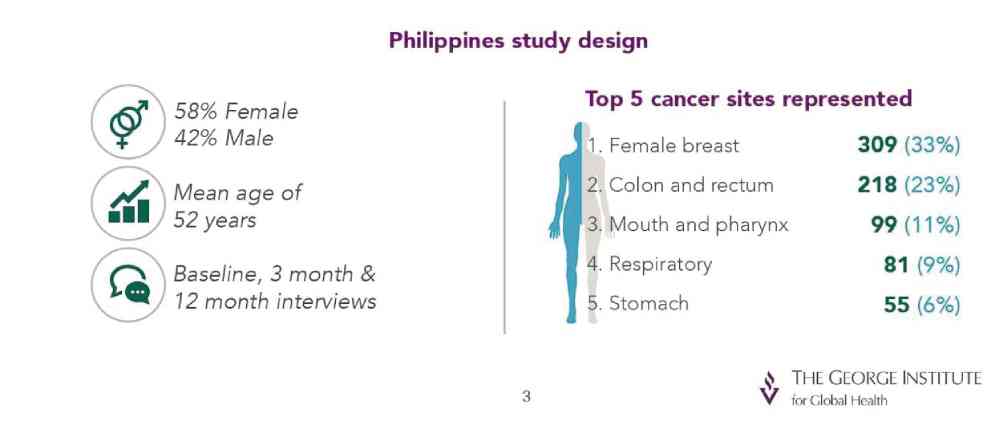
The study represented 909 Filipino patients with a mean age of 52 years. Of these patients, 59 percent were females and 75 percent were married.
Patients who had higher education were 40.5 percent; secondary, 36 percent; primary, 23 percent; and no education, 0.5 percent.
Those who were household heads were 46 percent; spouses of the head, 32.5 percent; offspring, 13 percent; parent, 3.5 percent; others, 6 percent.
Breast was the most common cancer site (one-third or 33 percent), followed by gastrointestinal tract (23 percent) and head and neck (11 percent). Next were respiratory (9 percent), hematologic (6 percent) and other cancer sites (18 percent).
A subanalysis of the Action study called Philippine Costs in Oncology (Peso) study showed these findings:
Disease and treatment
- Breast cancer patients in the country had the highest incidence of complete remission. They however had the highest percentage of financial catastrophe.
- Thirty-six percent of patients died within a year of diagnosis. Respiratory cancer has the highest incidence of death.
- All patients had planned treatment but only 79 percent of them received any treatment (surgery, radiotherapy, chemotherapy and hormone therapy). Very few patients were given biopharmaceutical drugs.
Quality of life
- Patients experienced problems related to mobility, personal care, usual activities, pain/discomfort and anxiety. These problems were observed to be on the rise three months and a year after diagnosis.
- Many patients shifted to elementary occupation (simple and nonskilled jobs) or lost time in house and paid work.
- Decrease in proportion of having full-time work (defined as 40 hours work per week) from baseline to month 12. The number of those who were not working increased from 53 to 80 percent a year after cancer diagnosis.
- Patients needing assistance for daily activities increased across time. At baseline, a patient needed an average five hours of support from caregivers such as spouses, children and friends. The time of caregiver support increased to 8 hours on month 3 and 10 hours on month 12.
- Cancer had an unfavorable effect on 41 percent of caregivers at baseline; increased to 49 percent at month 3; and 79 percent at month 12. They lost time in work, social activities and school.
- Those belonging to the low- and middle-income groups who were in advanced stages were vulnerable to poor survival.
- Patients with respiratory cancer had the highest incidence of anxiety and depression.
Financial catastrophe
- Patients experienced economic hardships. They asked financial assistance from family and/or friends, used savings, took out loans, sold assets and resort to other financial assistance.
- At 12 months, patients did not buy medicines or did not attend medical appointments. They prioritized food and shelter.
- Out-of-pocket health expenditure is higher than the annual family income. This includes hospital stay, medicines, traditional medicines and other costs (for example, medical supplies, food and transportation).
- Breast cancer patients had the highest incidence of financial catastrophe, followed by patients with gastrointestinal cancer.
- Many patients belonged to the lower-income group, earning between P51,500 and P103,000 per annum. Forty percent had no health insurance. Having health insurance however did not significantly predict survival or financial catastrophe.
- Those who were in the upper-income bracket had lower risk of financial catastrophe. Patients belonging to the low- and middle-income groups experienced financial catastrophe even when receiving only at least one planned treatment (one cycle of chemotherapy or one-week radiotherapy sessions).
- Less than 20 percent and less than 10 percent of the treatment were paid for by the government and private insurance, respectively. Government insurance (PhilHealth) covers only 11 percent of the total health expenditures.
- Out-of-pocket expenses increased by 71 percent three months after diagnosis. They take up 60 percent of the total health expenditures.
Conclusion
The Peso study showed that 56 percent suffered financial catastrophe a year after being diagnosed with cancer; 36 percent of patients died after a year; and only 8 percent of patients remained alive without experiencing financial catastrophe.
In the Philippines, therefore, cancer must be recognized and prioritized, and be seen as a national health issue affecting families, the society and the economy (loss of productivity for both patients and caregivers). There is an immediate and clear need to prioritize cancer to improve survival rates and reduce the financial burden.